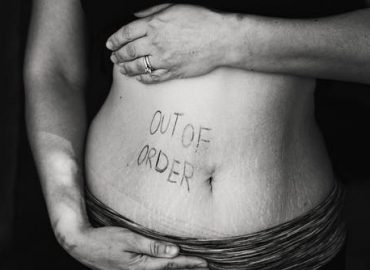
Tag: Inflammatory bowel disease
Gastrointestinal complaints are among the most common in health care.
There is a relationship between unfriendly bacteria in the gastrointestinal tract and a multitude of health issues in the gastrointestinal tract. The gastrointestinal tract house 100 trillion cells, more then all the stars in the sky! A major part of you immune and nervous system resides in the gastrointestinal tract. Therefore, if there is an imbalance in the bacterial balance in the gastrointestinal tract, one is more susceptible to autoimmune diseases, fatigue, irritable bowel syndrome, inflammations, food sensitivities, nutritional deficiencies and intestinal permeability (also known as “leaky gut”).
A diet rich in fiber allows the beneficial bacteria in the gastrointestinal tract to break down the fiber into short chain fatty acids. These short chain fatty acids are fuel for the intestinal enterocytes, which are the cell lining in the gut.
Stool analysis is an invaluable non-invasive diagnostic assessment that allows the practitioner to objectively evaluate the status of beneficial and imbalanced microorganisms.
Antimicrobial susceptibility testing to prescriptive and natural agents is also performed for non-desirable organisms which allows for a targeted treatment.
Comprehensive Stool Analysis w/Parasitology x 3
CGastrointestinal complaints are among the most common in medical care. This comprehensive profile helps pinpoint the causes of gastrointestinal symptoms and chronic systemic conditions, and measures key markers of digestion, absorption and inflammation. Using growth-based culture, the standard of practice in clinical microbiology, as well as sensitive biochemical assays and microscopy, this thorough stool test evaluates the status of beneficial and pathogenic microorganisms including aerobic and anaerobic bacteria, yeast and parasites.
Detailed Information
The Comprehensive Stool
Analysis with Parasitology x1, 2, or 3 is an invaluable non-invasive diagnostic
assessment that permits practitioners to objectively evaluate the status of
beneficial and imbalanced commensal bacteria, pathogenic bacteria, yeast/fungus
and parasites. Precise identification of pathogenic species and susceptibility
testing greatly facilitates selection of the most appropriate pharmaceutical or
natural treatment agents.
Important information regarding the efficiency of digestion and absorption can
be gleaned from the measurement of the fecal levels of pancreatic elastase
(pancreatic exocrine sufficiency), fat, muscle and vegetable fibers, and
carbohydrates. Inflammation can significantly increase intestinal permeability
and compromise assimilation of nutrients. The extent of inflammation, whether
caused by pathogens or inflammatory bowel disease (IBD), can be assessed and
monitored by examination of the levels of biomarkers such as lysozyme,
lactoferrin, white blood cells and mucus. These markers can be used to
differentiate between inflammation associated with potentially life-threatening
inflammatory bowel disease (IBD), which requires lifelong treatment, and less
severe inflammation that can be associated with irritable bowel syndrome (IBS)
which is frequently due to the presence of enteroinvasive pathogens.
Lactoferrin is only markedly elevated prior to and during the active phases of
IBD, but not with IBS. Monitoring fecal lactoferrin levels in patients with IBD
can therefore facilitate timely treatment of IBD, and the test can be ordered
separately. Since the vast majority of secretory IgA (sIgA) is normally present
in the GI tract, where it prevents binding of pathogens and antigens to the
mucosal membrane, it is essential to know the status of sIgA in the gut through
stool testing. sIgA is the only bona fide marker of humoral immune status in
the GI tract.
Cornerstones of good health include proper digestion of food, assimilation of
nutrients, exclusion of pathogens and timely elimination of waste. To obtain
benefits from food that is consumed, nutrients must be appropriately digested
and then efficiently absorbed into portal circulation. Microbes, larger-sized
particles of fiber, and undigested foodstuffs should remain within the
intestinal lumen. Poor digestion and malabsorption of vital nutrients can
contribute to degenerative diseases, compromised immune status and nutritional
deficiencies. Impairment of the highly specific nutrient uptake processes, or
compromised GI barrier function, as in “leaky gut syndrome,” can
result from a number of causes including:
· Low gastric acid production
· Chronic Maldigestion
· Food allergen impact on bowel absorptive surfaces
· Bacterial overgrowth or imbalances (dysbiosis)
· Pathogenic bacteria, yeast or parasites and related toxic irritants
· The use of NSAIDs and antibiotics
Impairment of intestinal functions can contribute to the development of food allergies, systemic illnesses, autoimmune disease, and toxic overload from substances that are usually kept in the confines of the bowel for elimination. After performing a stool test, efficient remediation of GI dysfunctions incorporates a comprehensive guided approach that should include consideration of elimination of pathogens and exposure to irritants, supplementation of hydrochloric acid, pancreatic enzymes and pre- and probiotics, and repair of the mucosal barrier.
Crohn Disease
Your digestive tract is the path that food takes through your body after you eat it. Food goes from your mouth (eating) to your anus (passing stool). Your intestine is the long tube in your digestive system that connects your stomach to your anus. It digests food and absorbs nutrients.
You have a small intestine and a large intestine. The small intestine, or small bowel, is very long with many coils. The large intestine, also called the colon or large bowel, is shorter and wider. Crohn disease is long-term inflammation in your intestines. Intestines are also called “bowels,” so Crohn disease is one of the two diseases called inflammatory bowel disease. The other inflammatory bowel disease is ulcerative colitis.
Omega-3 Fish Oil Supports Heart, Pain, and Autoimmune Inflammation
Omega-3 fish oil treats the following:
- High Blood Pressure
- High Cholesterol
- Chronic Pain
- Arthritis
- Inflammatory Bowel Disease
- Eczema
At Hunt Naturopathic Clinic we provide the care associated with the treatment of the above conditions which includes correct diagnostic assessment and treatment.
Heart Health
Studies have shown that a diet supplemented with omega-3 fish oil helps lower high blood pressure. In addition, omega-3 has been shown to reduce triglyceride levels by a net of about 50% compared with placebo [1]. And furthermore, patients who combined omega-3 fish oil with cholesterol lowering medication reported a net 23% decrease in their triglyceride levels [2].
Chronic Pain
Chronic pain can severely limit your mobility and lifestyle. Omega-3 fish oil has been shown to alleviate problems such as nonspecific neck and back pain, rheumatoid arthritis, pain associated with dysmenorrhea (painful periods), ankylosing spondylitis, and more [3].
Arthritis
Currently, Health Canada recommendations state that fish oil supplements reduce the pain of rheumatoid arthritis in adults when combined with traditional therapies [4]. Studies also suggest that supplementing with omega-3 for over 3 months can result in a notable reduction in the amount of arthritis medication that patients required [5].
Inflammatory Bowel Diseases
Patients who suffer from inflammatory bowel diseases such as ulcerative colitis and Crohn’s have taken part in trials using fish oil as part of their treatment. Results from these trails show not only a benefit from supplementation [6], but also that omega-3 may reduce steroid doses needed during treatment [7].
Eczema
Supplementing with omega-3 fish oil has the potential to result in improvements in the clinical features of eczema, such as scaling and itching [8]. Studies also confirm that taking fish oil during pregnancy may reduce the risk of the child developing eczema during their first year of life [9]
Book your appointment today! Click Here!